Motion-Processing Deficits Linked to Impaired Cognitive Function in Schizophrenia - Psychiatry Advisor

Investigators examined motion-processing deficits in the etiology of schizophrenia and attenuated psychosis.
Impaired motion processing in patients with schizophrenia is associated with deficits in cognitive and emotion detection processes, per study data published in The American Journal of Psychiatry.
Patients with schizophrenia (n=63) and patients with attenuated psychosis (n=32) were recruited from the Nathan Kline Institute for Psychiatric Research and the New York State Psychiatric Institute at Columbia University in New York City. Healthy volunteers of similar age to the schizophrenia group (n=44) and healthy volunteers of similar age to the attenuated psychosis group (n=23) were recruited from the surrounding communities.
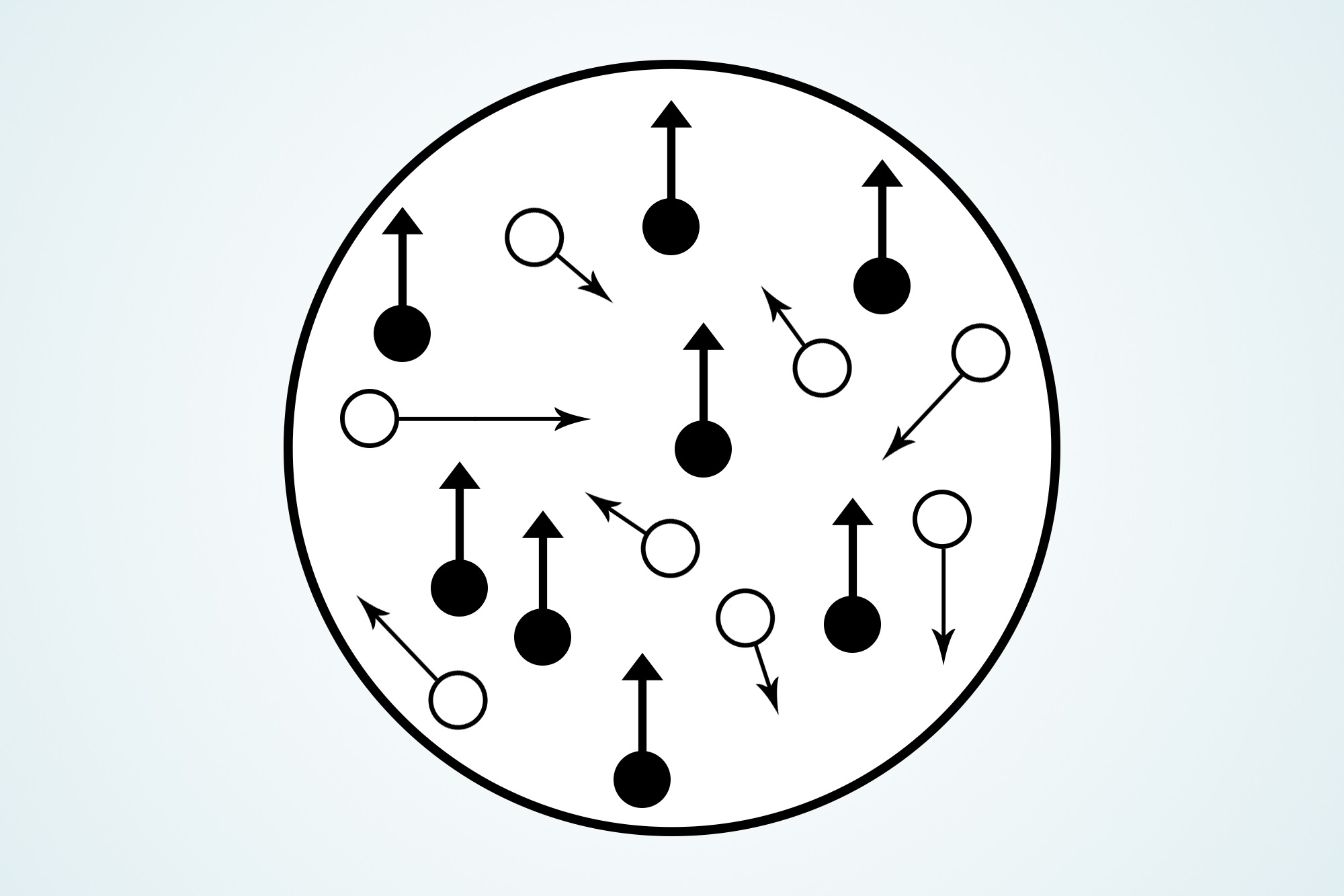
Participants responded to 3 visual simulation paradigms: behavioral, electroencephalogram (EEG), and functional magnetic resonance imaging (fMRI) methods. For the behavioral motion discrimination task, participants were exposed to random dot kinetograms and cued to describe in which direction the dots moved (left or right). For the EEG paradigm, participants were instructed to fixate on a visual stimulus and respond using a button press when the stimulus dimmed slightly; EEG activity was recorded continuously from 64 electrodes during the task. Finally, for the fMRI paradigm, low-contrast concentric rings were presented either as stationary or moving, after which participants indicated perception of the dimming event with a button press.
Psychiatric symptoms were assessed in clinical subjects using the Positive and Negative Syndrome Scale and the Scale of Prodromal Symptoms. General neuropsychological function and face emotion recognition was also assessed in the 2 patient groups per the Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery (MCCB) and the Penn Emotion Recognition Task, respectively.
Behavioral motion sensitivity differed significantly between clinical participants and control participants (P <.001), with significant performance reductions observed in patients with schizophrenia (P <.001) and patients with attenuated psychosis (P <.01) compared with their age-matched controls.
Per EEG data, significant between-group differences in motion-evoked (delta) activity existed for both the schizophrenia group (P =.008) and the attenuated psychosis group (P =.001) compared with age-matched healthy control participants; however, for stimulus-onset (theta) responses, clinical participants did not differ significantly from healthy control participants overall.
During fMRI scanning, correct detection of dimming events did not differ significantly between patients with schizophrenia (79%) and healthy control participants (87%) (P =.581); however, activation in the mid-temporal cortex (P <.015), middle occipital gyrus in the left hemisphere (P <.001), and right pulvinar of the thalamus (P <.001) in response to moving compared with stationary stimuli was substantially reduced in patients with schizophrenia compared with control participants.
Across both clinical subject groups, reduced delta activity correlated with lower composite scores on the MCCB (P =.001) and lower scores on the visual learning domain (P <.001), the attention/vigilance domain (P =.024), and the speed of processing domain (P =.001). Face emotion recognition scores were substantially poorer in individuals with attenuated psychosis who transitioned to schizophrenia during the study period compared with individuals who did not (P =.045).
This study underscores the salience of motion-processing deficits in the etiology of schizophrenia and attenuated psychosis. In addition, sensory-level visual dysfunction may "predate [schizophrenia] onset," per impairments observed in individuals with attenuated psychosis who later transitioned to schizophrenia.
Reference
Martínez A, Gaspar PA, Hillyard SA, et al. Impaired motion processing in schizophrenia and the attenuated psychosis syndrome: etiological and clinical implications [published online October 03, 2018]. Am J Psychiatry. doi:10.1176/appi.ajp.2018.18010072
https://ift.tt/2TV9Swa
Comments
Post a Comment