Valacyclovir Fails to Treat Herpes Simplex Virus-Type 1 in Schizophrenia - Psychiatry Advisor

Valacyclovir failed to significantly improve any of the cognitive indices, symptom or functioning measures.
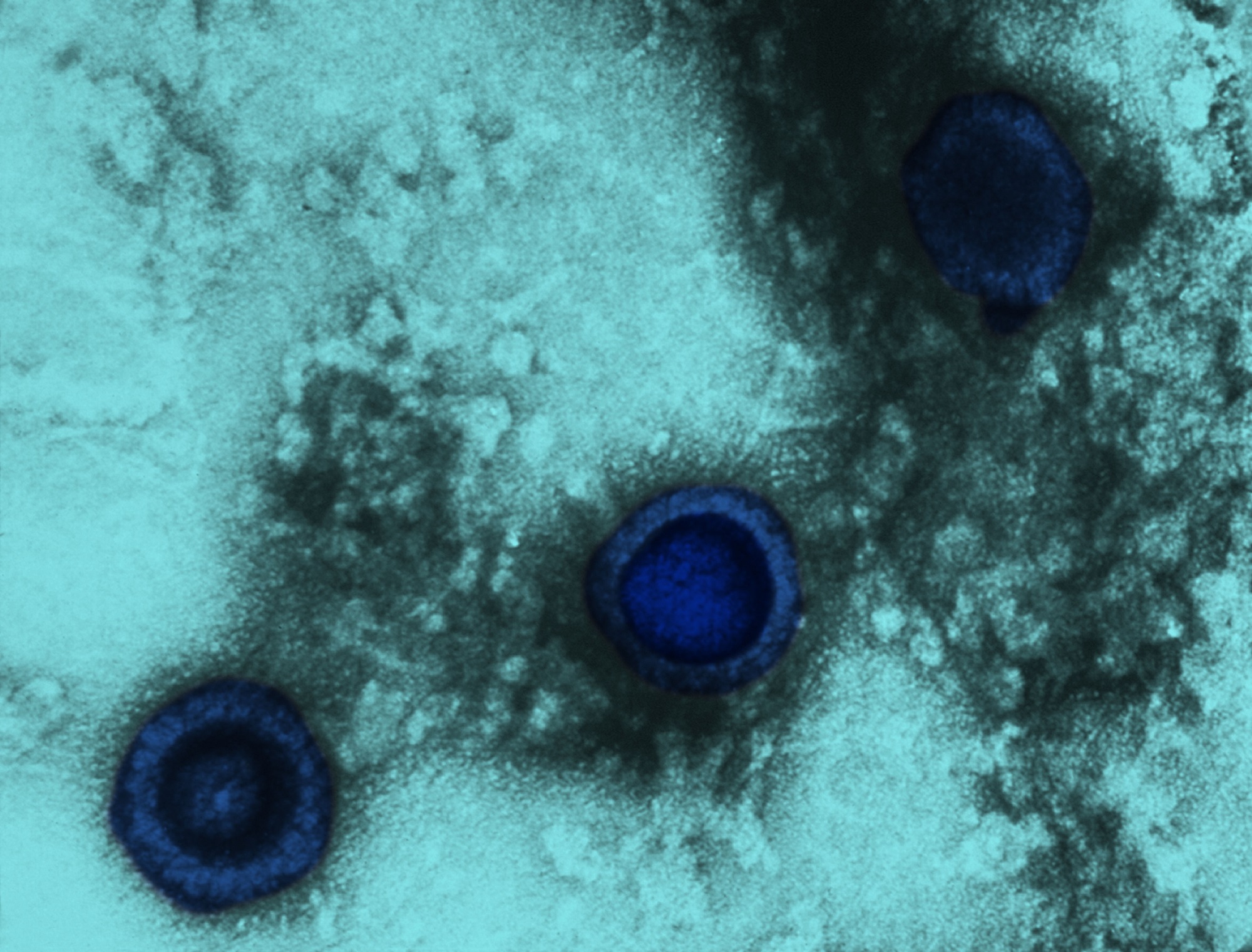
According to a study recently published in Schizophrenia Research, valacyclovir failed to improve working and visuospatial memory in individuals with herpes simplex virus-type 1 (HSV-1) and schizophrenia. Researchers further suggested that the presence of HSV-1 might be a clinical indicator of a more acute case of schizophrenia.1
Structural and functional brain changes are associated with HSV-1 infections in schizophrenia making for a strong case for considering antiviral medication trials in schizophrenia. Valacyclovir is a highly effective and relatively safe treatment for HSV-1 infection. However, it is only effective during the activated stage of viral replication, not for dormant infections.
In a study by Prasad et al, valacyclovir was associated with improvement in visual learning, and working and verbal memory when compared with placebo.2 However, this study had a small size with only 24 participants. So, researchers in this current study wanted to further characterize the clinical profile of HSV-1 positive vs HSV-1 negative individuals with schizophrenia and replicate the treatment results with a larger sample.
This double-blind study included 170 participants with schizophrenia, 74 of whom had confirmed HSV-1 and 96 of whom were HSV-1 negative (VISTA; ClinicalTrials.gov identifier: NCT02008773). Participation in this study took place at 12 sites in the United States, and participants were between the ages of 18 and 40 with a diagnosis of schizophrenia, schizophreniform, or schizoaffective disorder by DSM IV-TR criteria. Verbal and working memory comprised the study's primary endpoints.
As part of a 16-week efficacy trial, participants were randomly assigned 1:1 to valacyclovir 1.5 g twice daily or placebo. Measurements of function and cognition were performed at weeks 0, 8, and 16, while symptoms were assessed at weeks 0, 4, 8, 12, and 16. A mixed model analysis of covariance was utilized to investigate these data.
Several trends distinguished the HSV-1 positive group compared with the HSV-1 negative group: they were fewer men (P =.003), older (P <.001), had been ill for longer (P =.009), showed a greater number of symptoms (P =.016), had a lower quality of life (P =.035), and demonstrated poorer working memory via the letter-number sequencing test (P =.046) suggesting that HSV-1 infection may represent a subgroup of greater illness severity.
Valacyclovir failed to demonstrate significant treatment effects on the two primary cognitive outcome measures: the MATRICS Consensus Cognitive Battery working memory composite and visuospatial memory scores. Other cognitive, symptom and functional measures were not improved by valacyclovir.
Despite many similar methodological features including valacyclovir dose, treatment duration, and sample characteristics, this study failed to replicate the findings from the Prasad et al study. In fact, another replication trial initiated by the Prasad investigators showed findings similar to this study.3 However, Bhatia et al did report improvement in accuracy scores of emotional identification and discrimination,3 which is a finding that will need further replication.
The authors noted that HSV-1 viruses may have been in the predominately dormant state in this study and therefore resistant to valacyclovir, since this medication is only effective when the virus is in the activated state.
“It may be important to conduct future valacyclovir trials in subjects with clinical signs of activated virus and perhaps those with very high HSV-1 antibody titers,” concluded the researchers.
References
- Breier A, Buchanan RW, D'Souza D, et al. Herpes simplex virus 1 infection and valacyclovir treatment in schizophrenia: Results from the VISTA study [published online November 23, 2018]. Schizophr Res. doi: 10.1016/j.schres.2018.11.002
- Prasad KM, Eack SM, Keshavan MS, Yolken RH, Iyengar S, Nimgaonkar VL. Antiherpes virus-specific treatment and cognition in schizophrenia: a test-of-concept randomized double-blind placebo-controlled trial. Schizophr Bull. 2013;39(4):857-866.
- Bhatia T, Wood J, Iyengar S, et al. Emotion discrimination in humans: Its association with HSV-1 infection and its improvement with antiviral treatment. Schizophr Res. 2018;193:161-167.
http://bit.ly/2CIuVLO
Comments
Post a Comment