Columbia Just Launched the Center for Precision Psychiatry and ... - zuckermaninstitute.columbia.edu
Psychiatric medicine is on the cusp of a new era of more precise and effective diagnosis and treatment. With its launch earlier this week of the Stavros Niarchos Foundation Center for Precision Psychiatry and Mental Health, Columbia University is combining its strengths in neuroscience research and clinical innovation to hasten the arrival of this next generation of psychiatric diagnosis, treatment and care.
To learn more about the new center and what precision psychiatry could mean for us all, we caught up with Dr. Joseph Gogos, MD, PhD, a co-director of the new center whose own research has focused on the biological basis of schizophrenia. His codirectors are Drs. Sander Markx and Steven Kushner, both physician-scientists in the Department of Psychiatry at Columbia's Vagelos College of Physicians and Surgeons and New York State Psychiatric Institute. Dr. Gogos is also a principal investigator at Columbia's Zuckerman Institute and a professor of physiology & cellular biophysics, neuroscience and psychiatry at Columbia's Vagelos College of Physicians and Surgeons.
What driving needs in science and society does Columbia's new Center for Precision Psychiatry and Mental Health address?
Approximately one in four people experiences mental illness each year, and close to 1 billion people in the world live with a diagnosable mental disorder. Mental illness can have a significant impact on an individual's overall health and well-being. It is one of the leading causes of disability as well as premature death due to preventable physical ailments such as cardiovascular disease, diabetes, and other chronic health conditions. Suicide is the second leading cause of death among young people. People with mental illness also experience widespread human-rights abuses, discrimination and stigmatization in many areas of their lives, including employment, healthcare, housing and education. This discrimination can limit access to essential resources and services, which can exacerbate mental health conditions.
Despite the progress made in recent years, health systems worldwide have not yet effectively responded to the financial, medical, and societal burdens of mental disorders. The COVID-19 pandemic and the unprecedented mental health crisis it revealed has exposed the fragility of mental healthcare systems. It is more important than ever to invest in mental health research in bold and visionary ways that can leverage a rigorous scientific approach into new treatments for mental disorders that are safe and effective. This will help bring us the precision psychiatry that stands to benefit so many people.
Define the term "precision psychiatry."
Precision psychiatry is an emerging field that aims to improve the accuracy and effectiveness of psychiatric diagnosis and treatment based on a patient's underlying disease etiology.
"Precision" as a modifier to the word "psychiatry" is defined as "adapted for accuracy and exactness" and therefore implies that the latter is founded on rigorous measurement. Unlike medical disciplines such as cardiology and neurology, however, psychiatry does not routinely use exact measurements and data such as lab tests and MRI scans to track the equivalent of vital signs and their molecular and cellular reflections in the blood and peripheral tissues. Instead psychiatry relies heavily on intuition and experiential trial and error. In that regard, the word "precision" expresses not a reality, but a vision, a long-awaited ideal that, if fulfilled, will forever transform psychiatry and people's lives. Turning this precision ideal into reality is an ambitious task, but the timing and the odds for successfully carrying it out have never been more favorable.
Co-directors of the Center for Precision Psychiatry and Mental Health: from left to right, Sander Markx, Joseph Gogos and Steven Kushner.
What do you hope to accomplish with the new center? Who will benefit?
Personalized care has long been the hallmark of psychiatry, and it is based on trust and rapport between patient and physician. This relationship is vital for placing and treating the disease in the context of each patient's individual resiliency as well as their lifestyles and environmental circumstances.
The new center's goal is to provide the tools for personalized psychiatric care to become precise at a high level of biological exactness. We want this measurement-anchored approach to become the basis for improving psychiatric medicine's efficiency, safety and cost-effectiveness, reducing its side effects and making it more inclusive and equitable.
Our vision is to eventually reduce the burden of mental illness. At the same time, we are committed to fighting social inequities in mental healthcare by ensuring that the very best innovations in medicine are available to everyone, regardless of racial, ethnic, religious or socioeconomic background.
Why is foundational research so essential to this effort?
The recent history of cancer medicine is instructive here. In oncology, the practice of diagnosing and defining malignancies by their bodily location (e.g., breast cancer or lung cancer) had been counterproductive and had stalled progress in cancer outcomes for years. The awareness that cancer is a molecular disease caused by specific mutations in genes that regulate cell proliferation led to the profound insight that there are many different types of cancer defined not by location but by their molecular triggers. This allowed researchers in the past three decades to identify specific genetic mutations that drive the development of cancer, to develop targeted therapies that can block these mutations and to precisely predict treatment responses.
As with oncology, the endeavor of bringing precision to psychiatry rests solely on the evolving basic-science knowledge of the biological pathways involved in major mental illnesses. It builds on deciphering etiologies to target therapeutically accessible disease mechanisms; refining the classification of mental illnesses based on their neurobiological underpinnings rather than symptoms; finding measurable biomarkers or laboratory tests capable of guiding clinical diagnosis and treatment; and providing a baseline from which to evaluate each patient's recovery.
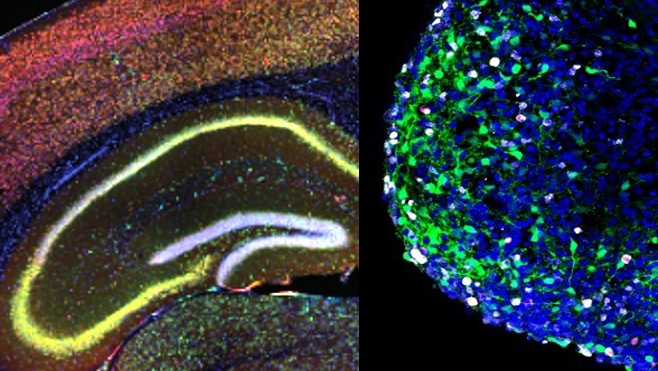
Pathways to precision psychiatry. The image on the left reveals a distribution (yellow) of a gene-quieting molecule in mouse brain cells engineered to have a genetic trait associated with schizophrenia. This manipulation leads to full restoration of a key cognitive deficit in the mice. The image on the right shows an organoid—a three-dimensional cell culture derived from brain cells of people with schizophrenia. These can serve as research models for studying the cellular bases of psychiatric conditions and for screening drug candidates. (Credit: Zuckerman Institute/Gogos lab)
How will you and colleagues translate the center's research into clinical and therapeutic practice?
The years from 2004 to 2013 were arguably "anni mirabiles," or wonderful years, for the enormous, decades-old challenge of deciphering the causes and mechanisms of major mental illnesses, such as schizophrenia. Over this decade, powerful molecular genetic technologies, along with advanced computational tools, offered the means to reveal individuals' genetic vulnerability to major mental illness. By studying the genetic material of affected families, a number of groups around the world, including our group and collaborators at Columbia, trailblazed this new era of knowledge, offering important insights into the genetic architecture of schizophrenia. Empowered by new and powerful neuroscience techniques, and mouse models genetically modified to carry psychiatric disease genes, we also started identifying malfunctioning neuronal circuits that may prove essential in establishing novel treatment strategies.
The new center is built upon this foundational knowledge. We expect to expand that knowledge base by accumulating massive data sets on genetics and medical records; employing new experimental and analytical approaches to disease models; and harnessing interdisciplinary expertise and perspectives from biologists, statisticians and clinicians. Precision-psychiatry clinical trials for disease mechanisms associated with the most strongly validated risk genes and biological mechanisms (such as autoimmunity) will be an important part of our mission. Those trials will be performed through the Department of Psychiatry and the New York State Office of Mental Health.
Our goal and mandate is to enable the rapid advent of new therapeutic and prevention approaches that will benefit individual patients (based on their unique genetic and pathophysiological traits) as well as groups of patients that share core etiologies.
What role will the Zuckerman Institute play?
Identifying new treatments for psychiatric disorders is an inherently multilevel and multidisciplinary endeavor. Over the past several years, efforts from my group to decipher the neurobiological underpinnings of mental disorders greatly benefited from our interactions with a diverse team of extraordinary scientists at the Zuckerman Institute and use of cutting-edge neuroscience tools. We hope to expand and amplify such interactions and accomplish an integration and synergy between the extraordinarily successful mental health and neuroscience programs at Columbia University. With these collaborations, we expect to identify neural footholds from which we can uncover novel therapeutic targets and deliver highly effective personalized therapies.
How is the center different from existing organizations in the psychiatry and mental health research space?
There is simply no other place where these projects could be as effectively pursued than at Columbia University, because of the unique combination of knowledge, expertise and infrastructure of Columbia psychiatry and neuroscience communities. In addition, Columbia is home to the New York State Psychiatric Institute, which directly connects clinical care and research at Columbia to a massive New York State program in psychiatric diseases through the New York State Office of Mental Health. This connection affords the opportunity to engage mental health patients and their long-term clinical records as a means of advancing clinical care, translational neuroscience and genomic medicine.
How did the new center progress from a glimmer in your and your colleagues' eyes to its launch earlier this month?
A center that advances foundational psychiatric research and translating it into treatments has been part of the university's collective vision, and something that I have personally dreamed of. The center was conceptualized in its current form in the fall of 2019 during a trip I took to Athens, Greece, through discussions with a visionary Greek mental health advocate, former prime minister Antonis Samaras. This led to a series of meetings with the Stavros Niarchos Foundation (SNF), a philanthropy founded in 1996 that works in Greece and around the world. SNF derives its mission from founder Stavros Niarchos´s commitment to Greece and Hellenism, as well as his keen interest to improve the lives of people worldwide by supporting causes in the fields of health, social welfare, education and in arts and culture.
In the midst of COVID-19, Dr. Sander Markx, a codirector or our new center, and I had many meetings with the SNF leadership and scientific advisory board. These included truly inspiring discussions with SNF co-president Andreas Dracopoulos, whose passion to fight mental illness and promote mental health worldwide was the driving force behind the creation of the new center. Also helping us hone the details of our endeavor were input and guidance from Panos Papoulias, Chief Operating Officer of SNF, and Elianna Konialis, SNF's Health Initiative Grant Manager. Zuckerman Institute founding codirector, Richard Axel, MD, and former institute co-director Rui Costa, DVM, PhD, added to the vision behind the center, as did Tom Maniatis, PhD, a principal investigator at the Zuckerman Institute and director of Columbia's Precision Medicine Initiative, a related cross-departmental effort. Columbia President Lee Bollinger was instrumental in helping us cross the finish line.
The concept for the Center for Precision Psychiatry and Mental Health metamorphosed into a reality in the summer of 2022 when the SNF announced in Athens a gift of $75 million to establish the center. And on April 25, 2023, Columbia University officially launched the center.
The origins of precision medicine date back to ancient texts of Hippocrates and his students, who recognized that humans have individual differences and do not all respond similarly to treatment. In that respect, I am delighted that SNF, a foundation with strong Greek roots, makes such a difference in the lives of those struggling with mental health challenges by helping to promote the ideals of precision medicine in psychiatry.
Comments
Post a Comment