Comorbidity of Anorexia Nervosa and Schizophrenia: A Case Study ... - Psychiatric Times
MartaKlos/AdobeStock

SPECIAL REPORT: CLINICAL COMPLICATIONS OF COMORBIDITIES
Eating disorders, particularly anorexia nervosa (AN), are underdiagnosed and often go undetected in populations with primary psychotic disorders. Most of the literature that examines eating disorders in populations with severe mental illness has focused on binge-eating disorders. This is likely caused by the increased appetite often seen in patients who are treated with antipsychotic medications.
There are fewer investigations that consider the co-occurrence of schizophrenia and AN. This may be because of the difficulties in differentiating reduced food intake secondary to mood and psychotic symptoms from those that can be attributed to a primary eating disorder. This has potentially deleterious consequences given that AN has the highest mortality rate of all psychiatric diagnoses and is also one of the most difficult diagnoses to manage.1
For these reasons, it is important that clinicians are able to both detect and comfortably manage primary eating disorders in patients with severe mental illness. Recognition and cotreatment are particularly important in inpatient settings, where clinicians are more likely to encounter patients who are severely underweight.
Prevalence and Challenges
The incidence of AN in the general population is approximately 1% to 4%.2,3 Symptoms of AN are seen in up to 13% of patients with schizophrenia, and some studies suggest a genetic link between the disorders.2-5 Although schizophrenia and AN are 2 distinct psychiatric disorders, several points of overlap can make it difficult for physicians to distinguish between them when they are present in the same individual.
For example, traits such as the obsessionality seen in patients with AN can be mistaken for preoccupation in patients with schizophrenia.6-8 Similarly, the restrictive eating patterns that are prominent in those with AN can be misattributed to depression, somatic preoccupation, delusional thoughts (eg, thinking the food is poisoned), or failure to thrive in older individuals. Thus, despite the relatively frequent co-occurrence between schizophrenia and AN, unique factors complicate the process of detecting the 2 disorders in the same individual.
Clinical Impact
There is a need for greater awareness and diagnostic sophistication when approaching the patient with schizophrenia who presents with restrictive eating; however, there is limited literature on the co-occurrence of the disorders, particularly in older adults. AN is a notoriously difficult disorder to manage and requires a specialized treatment plan that involves a multidisciplinary team of clinicians including psychiatrists, therapists, and dietitians.9,10 Patients with schizophrenia whose AN goes undetected may not receive adequate treatment for their disordered eating.
A case of AN in a 74-year-old woman with longstanding schizophrenia is presented herein. This case is unique given the patient's advanced age and long history of distinct psychotic and eating disorder pathology. The goal of this case presentation is to add to the small body of literature regarding this topic to provide guidance for diagnostic clarification for inpatient management of a population that is particularly difficult to treat and requires a unique and targeted approach.
Case Study
"Magda," a 74-year-old woman with a history of schizophrenia with persistent auditory hallucinations at baseline presented to the Comprehensive Psychiatric Emergency Program after a yearlong decline mentally and physically. She had weight loss and multiple somatic complaints, including palpitations, dizziness, and nausea. Magda had been partially adherent to medications, taking only half of her prescribed antipsychotic dose for fear that it was the cause of her palpitations.
Magda stated that she had poor self-care, low mood, insomnia, fatigue, poor appetite, and suicidal ideation without method, intent, or plan. She presented as anxious, somatically preoccupied, and psychomotor slowed. Her body mass index (BMI) was 15.2. Collateral information obtained from her family suggested that the patient was experiencing command auditory hallucinations to not eat. She had lost nearly 15 lb from her baseline weight over the past year. The patient was admitted voluntarily for psychotic decompensation and a major depressive episode.
Once on our inpatient unit, the patient was started on and up-titrated to optimal doses of quetiapine and fluoxetine with moderate improvement in symptoms. Magda's affect brightened, and she reported a reduction in depressive symptoms as well as improvement in the derogatory nature of her auditory hallucinations. Many of her somatic preoccupations remitted, although she remained preoccupied by gastrointestinal symptoms she experienced after meals, including bloating, gas, headache, and nausea. She rarely completed her meals, and her weight gain plateaued after several weeks following admission.
The patient's postmeal somatic preoccupations and inadequate food intake remained present even as she approached her psychiatric baseline. Magda denied most depressive symptoms as well as derogatory or command auditory hallucinations at week 6 of admission. She stated she had a good appetite but felt full after finishing the salad and vegetable portions of her meals. Magda denied command auditory hallucinations to restrict her food intake. She demonstrated poor insight into her malnourished state and requested to be discharged because her mood and psychotic symptoms had improved.
Upon further evaluation, Magda described restrictive eating patterns since her early 20s, which predated the onset of psychotic symptoms. She described her diet at home, which included boiling lettuce and watercress and drinking the water, eating a single bowl of oatmeal throughout the day, eating a salad at night, and often supplementing food with tea. She expressed concerns about her shape and weight, referring to her legs as "chubby" and perceiving herself as overweight.
The treatment team amended Magda's goals to include restoring her weight and, with the help of a dietitian, incorporating a greater variety of foods into her diet. The patient was given a goal weight (5 lb from her weight at that time) that, once met, would indicate her readiness for discharge.
Efforts to carry out this treatment plan were met with frequent anger from Magda, who described the sensation of bloating she experienced from eating all of her meals as "torture." She perseverated on her meal portions, stating that she believed the treatment team was secretly giving her "triple portions" without her consent. She frequently argued with the treatment team, claiming that she felt there was no actual difference in size between her current weight and her last known normal weight, stating that they were "just different numbers." Magda's distress and preoccupation initially resulted in increased restriction during some meals, followed by an initial decrease in body weight.
Over the course of 4 weeks, Magda steadily improved in her ability to tolerate distress about weight gain, and her BMI increased from 15.2 on admission to 17.7, a total of 16 lb gained. She declined the treatment team's recommendation for residential placement and was discharged to a partial hospitalization program (PHP). She did not follow up for care with the PHP and was subsequently admitted medically for nursing home placement.
Discussion
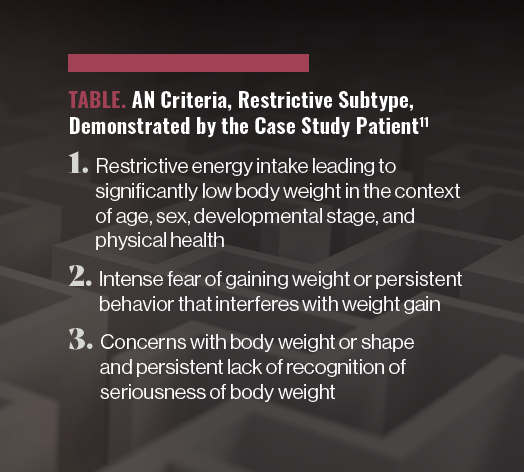
This older patient with schizophrenia in this case demonstrated all of the criteria for AN, restrictive subtype, including restrictive energy intake leading to significantly low body weight in the context of age, sex, developmental stage, and physical health; intense fear of gaining weight or persistent behavior that interferes with weight gain; and concerns with body weight or shape and persistent lack of recognition of seriousness of body weight (Table).11 This case is unique for several reasons.
Table. AN Criteria, Restrictive Subtype, Demonstrated by the Case Study Patient11
First, this patient had encountered countless medical and mental health professionals throughout her longstanding course of psychiatric illness without receiving a formal diagnosis or treatment for AN. Second, what was ultimately determined to be eating disorder psychopathology was initially mistaken to be explained by her depression and psychotic symptoms. Third, very few cases of comorbid schizophrenia and AN have been described in the literature, and most of the current evidence describes binge-eating behaviors as opposed to the restrictive eating patterns and body image concerns previously described.12-17 Finally, to our knowledge, co-occurring schizophrenia and AN have never been described in an older individual, with distinct psychopathology for both disorders extending back at least 50 years.
Diagnostic Clarification
It can be particularly challenging to identify disordered eating in older patients with comorbid psychiatric disorders. Without the current patient's body weight concerns and her extreme reaction to efforts to restore her weight, the treatment team could have mistaken the patient's presentation for failure to thrive (a state of global decline that includes weight loss, decreased appetite, poor nutrition, and inactivity, often accompanied by depression and malnutrition)18 following her improvement in psychotic symptoms. Additionally, patients with psychotic disorders often present with food refusal in the setting of psychotic decompensation.
We advocate for brief but more frequent screening for eating disorder pathology in patients with psychotic disorders who present with decreased food intake and weight loss. Screening tools available include the Eating Disorder Screen for Primary Care, Screen for Disordered Eating, and the SCOFF questionnaire.19 Asking patients about their concerns regarding body image and weight gain will likely be most informative, as it was in this case.
Recommendations for Management
Our recommendations for inpatient management are as follows. A goal weight should be determined either by growth curve trajectories (in younger patients) or by the last known normal weight. The goal weight should be shared with the patient. Meal plans should incorporate input from a registered dietitian, and the patient should meet with a dietitian at least weekly. Electrolytes including magnesium and phosphorous should be monitored on day 1, day 4, and weekly following initiation of weight restoration.
Increased privileges on the unit can be incorporated when certain weight goals are achieved. This was not used with our patient, given that her main motivating factor was discharge (as opposed to increased privileges). Patients should be weighed 1 or 2 times weekly, and we recommend that this weight be shared with the patient for transparency.
Weight restoration is notoriously difficult to achieve in patients with AN, so treatment teams should expect the weight restoration phase to last at least as long as, if not longer than, the time necessary to manage the patient's psychotic symptoms. Each of these treatment recommendations can be incorporated on most inpatient psychiatric units that have access to registered dietitian services.
Concluding Thoughts
Symptoms of AN are seen more frequently in patients with schizophrenia compared with the general population, yet AN and schizophrenia can be difficult to distinguish. This likely results in underdiagnosis of AN in patients with schizophrenia, despite the high mortality rate of AN compared with other psychiatric disorders, and the need for a specialized treatment approach.
We recommend more frequent and careful screening for eating disorders in patients with psychotic disorders who present with low weight. Patients with psychotic disorders who present with disordered eating should receive a specialized treatment approach from a multidisciplinary team of medical and mental health professionals as well as dietitians.
Dr Koljack (PGY-3) is a resident in the Department of Psychiatry at Columbia University Irving Medical Center, New York State Psychiatric Institute. Dr Holderness is an associate clinical professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons, New York State Psychiatric Institute.
References
1. Edakubo S, Fushimi K. Mortality and risk assessment for anorexia nervosa in acute-care hospitals: a nationwide administrative database analysis. BMC Psychiatry. 2020;20(1):19.
2. Kouidrat Y, Amad A, Lalau JD, Loas G. Eating disorders in schizophrenia: implications for research and management. Schizophr Res Treatment. 2014;2014:791573.
3. Morylowska-Topolska J, Ziemiński R, Molas A, et al. Schizophrenia and anorexia nervosa - reciprocal relationships. A literature review. Psychiatr Pol. 2017;51(2):261-270.
4. Zhang R, Larsen JT, Kuja-Halkola R, et al. Familial co-aggregation of schizophrenia and eating disorders in Sweden and Denmark. Mol Psychiatry. 2021;26(9):5389-5397.
5. Marucci S, Ragione LD, De Iaco G, et al. Anorexia nervosa and comorbid psychopathology. Endocr Metab Immune Disord Drug Targets. 2018;18(4):316-324.
6. Halmi KA, Sunday SR, Strober M, et al. Perfectionism in anorexia nervosa: variation by clinical subtype, obsessionality, and pathological eating behavior. Am J Psychiatry. 2000;157(11):1799-1805.
7. Anderluh MB, Tchanturia K, Rabe-Hesketh S, Treasure J. Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. Am J Psychiatry. 2003;160(2):242-247.
8. Vitousek K, Manke F. Personality variables and disorders in anorexia nervosa and bulimia nervosa. J Abnorm Psychol. 1994;103(1):137-147.
9. Crone C, Fochtmann LJ, Attia E, et al. The American Psychiatric Association practice guideline for the treatment of patients with eating disorders. Am J Psychiatry. 2023;180(2):167-171.
10. Muratore AF, Attia E. Current therapeutic approaches to anorexia nervosa: state of the art. Clin Ther. 2021;43(1):85-94.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition, Text Revision. American Psychiatric Association Publishing; 2022:381-387.
12. Yum SY, Caracci G, Hwang MY. Schizophrenia and eating disorders. Psychiatr Clin North Am. 2009;32(4):809-819.
13. Cinemre B, Kulaksizoğlu B. [Case report: comorbid anorexia nervosa and schizophrenia in a male patient]. Turk Psikiyatri Derg. 2007;18(1):87-91.
14. Miotto P, Pollini B, Restaneo A, et al. Symptoms of psychosis in anorexia and bulimia nervosa. Psychiatry Res. 2010;175(3):237-243.
15. Lobo CDA, Adame CV, Aparicio TJ, et al. Comorbid anorexia nervosa and schizophrenia. Eur Psychiatry. 2021;64(suppl 1):S243-S244.
16. Imran N, Rumesa F, Jamil F. Comorbid schizophrenia and anorexia nervosa in an adolescent male. Pak J Med Sci. 2018;34(5):1297-1299.
17. Daryani NE, T-Vakili S, Abdollahzade S. An association between anorexia nervosa and schizophrenia: a case report. Govaresh. 2011;16(2):139-143.
18. Robertson RG, Montagnini M. Geriatric failure to thrive. Am Fam Physician. 2004;70(2):343-350.
19. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for eating disorders in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA. 2022;327(11):1061-1067.
Comments
Post a Comment